 If you’re exploring options for dental implants or dealing with jawbone issues, you may have heard about a dental bone graft. This common procedure helps restore bone volume and density in the jaw, making it a key step for many patients seeking stable, long-lasting tooth replacements.
If you’re exploring options for dental implants or dealing with jawbone issues, you may have heard about a dental bone graft. This common procedure helps restore bone volume and density in the jaw, making it a key step for many patients seeking stable, long-lasting tooth replacements.
As a dentist, I often explain that a bone graft for teeth acts like a foundation repair—it rebuilds support where bone has been lost, so implants can thrive. In this guide, we’ll cover everything you need to know in a straightforward way.
Why Jawbone Health Matters Before Dental Implants
Your jawbone does much more than hold your teeth in place. It’s a living structure that requires constant stimulation from tooth roots to maintain its density and volume. When you chew, the pressure transmitted through your teeth keeps your jawbone strong and healthy—much like exercise keeps your muscles toned.
Here’s why jawbone health is critical:
Supporting Dental Implants
Dental implants are titanium posts that act as artificial tooth roots. They need sufficient bone thickness and height to anchor securely. Without adequate bone, implants can fail or become unstable over time.
Maintaining Facial Structure
Your jawbone supports the shape of your face. When bone loss occurs, it can lead to a sunken appearance, premature aging, and changes to your facial profile that make you look older than you are.
Preserving Oral Function
A healthy jawbone allows you to chew effectively, speak clearly, and maintain proper bite alignment. Bone loss can compromise all these functions.
The consequences of jawbone deterioration extend beyond cosmetics. You may experience difficulty eating certain foods, changes in how your remaining teeth fit together, and even jaw pain. This is why dentists often recommend bone grafting—not just for implant placement, but for overall oral health preservation.
Signs You Might Need a Bone Graft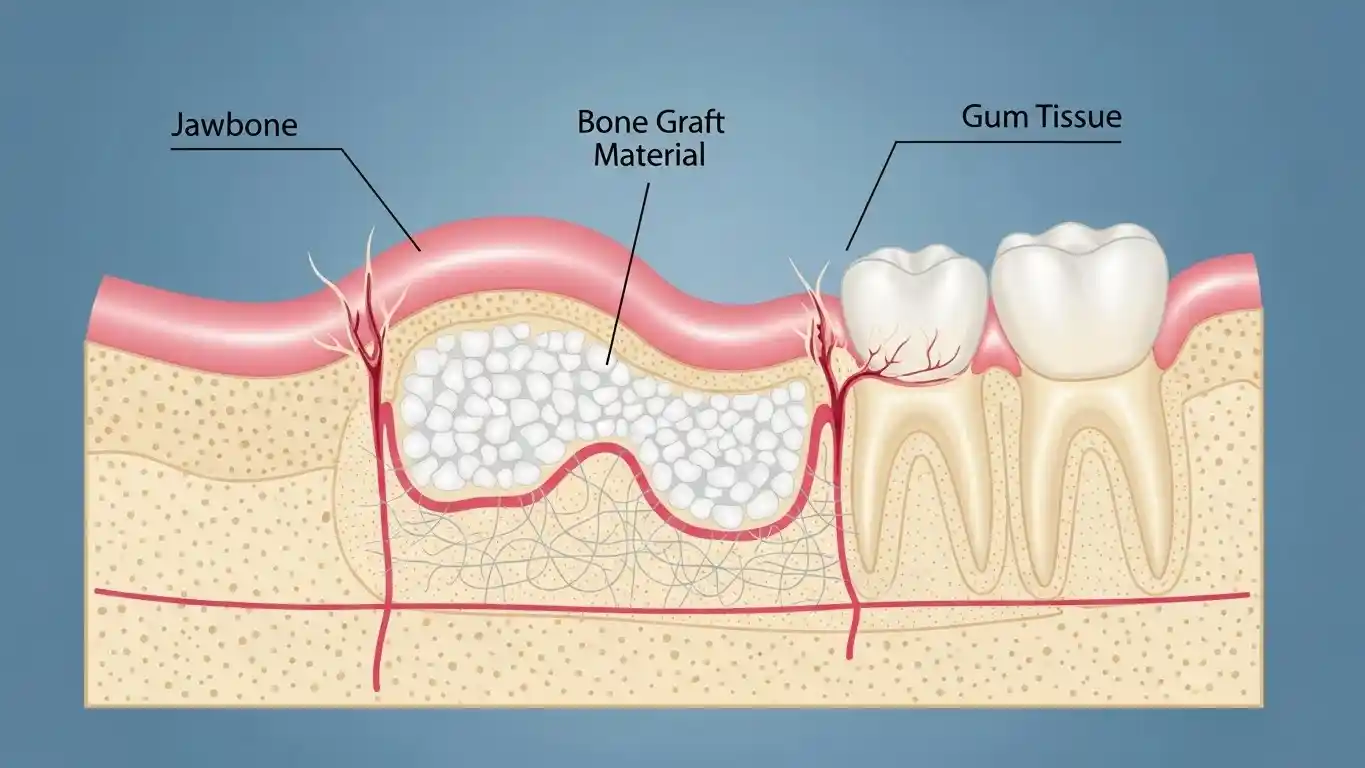
How do you know if you’re a candidate for a dental bone graft? Several situations commonly lead to the need for bone regeneration:
- Recent or Long-Term Tooth Loss: When you lose a tooth, the surrounding bone begins to deteriorate within the first year—and can continue shrinking over time
- Advanced Gum Disease: Periodontal disease doesn’t just affect your gums; it destroys the bone supporting your teeth
- Facial Trauma or Injury: Accidents that damage the jaw can result in bone loss that requires reconstruction
- Congenital Deficiencies: Some people are born with inadequate jawbone development in certain areas
- Previous Tooth Extractions: Especially if performed years ago without socket preservation techniques
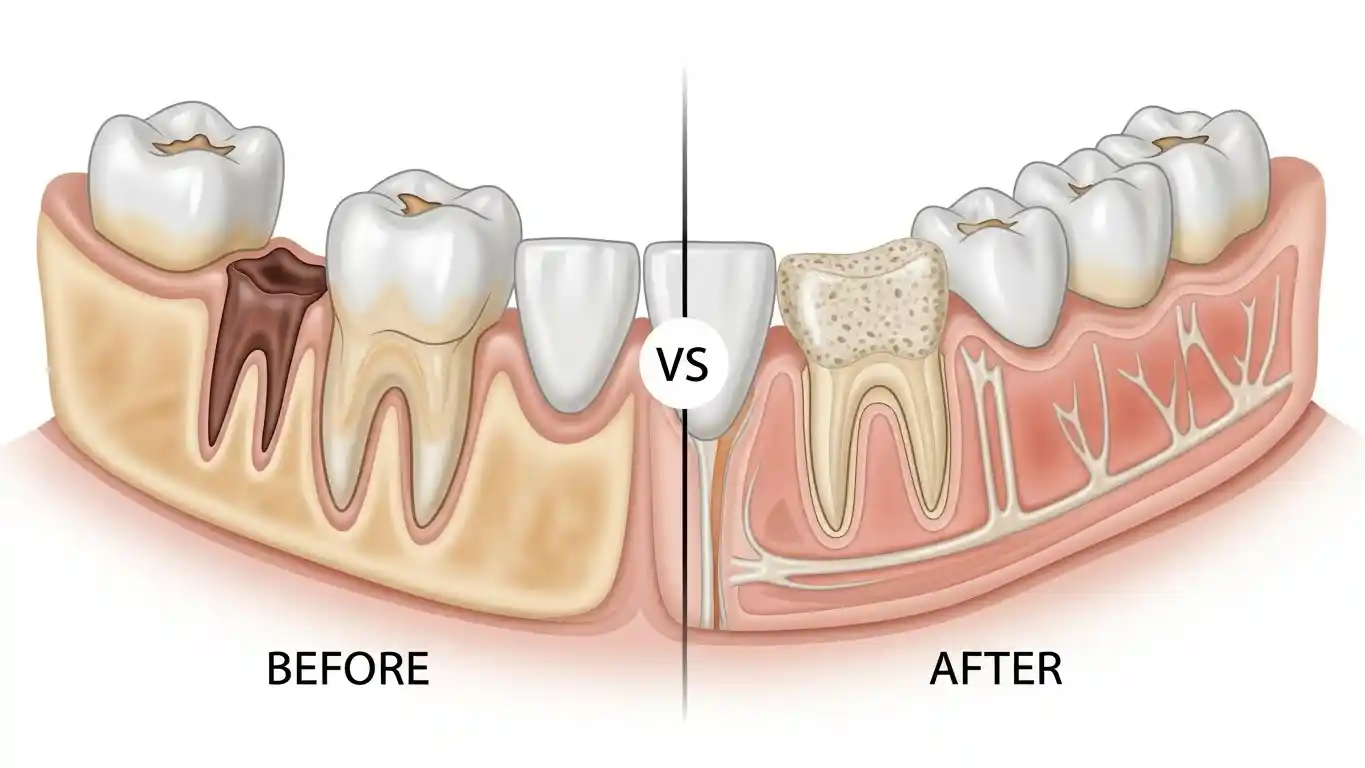
Understanding Bone Grafting: How It Works
The bone graft procedure might sound intimidating, but understanding the science behind it can ease your concerns and help you see why it’s such an effective solution.
The Science Behind Bone Regeneration
Dental bone grafting works by providing a scaffold—a framework that your body uses to build new bone. The graft material you receive serves as a foundation that stimulates your natural bone cells to grow and eventually replace the graft with your own healthy bone tissue.
This process, called osseointegration, happens gradually over several months. Your body recognizes the graft material as a surface where bone can form, and specialized cells called osteoblasts begin creating new bone tissue. Blood vessels grow into the area, bringing nutrients and supporting continued bone development.
Step-by-Step Bone Graft Procedure
Knowing what to expect during a bone graft procedure can significantly reduce anxiety. Here’s what typically happens:
Before Surgery: Your dentist will review your medical history, discuss anesthesia options, and may prescribe antibiotics to prevent infection. You’ll receive detailed pre-operative instructions about eating, drinking, and medications.
During the Procedure:
- Anesthesia Administration: Local anesthesia numbs the surgical area, though sedation options are available if you’re anxious or having extensive work done
- Incision: Your dentist makes a small incision in your gum tissue to expose the bone underneath
- Graft Placement: The bone graft material is carefully positioned where bone regeneration is needed
- Securing the Graft: A protective membrane may be placed over the graft to keep it in position and guide bone growth
- Suturing: The gum tissue is closed with stitches, which are typically dissolvable
Types of Dental Bone Grafts
Not all bone grafts are created equal. Your dentist will recommend the type that best suits your specific situation, considering factors like the amount of bone needed, the graft location, and your overall health.
Autografts: Using Your Own Bone
An autograft uses bone harvested from another area of your own body—typically your chin, jaw, hip, or shin. This is considered the “gold standard” by many dental professionals.
- Advantages: Since it’s your own tissue, there’s no risk of rejection, and autografts contain living bone cells that promote faster, more predictable healing. The success rate for autografts is exceptionally high.
- Considerations: The main drawback is requiring a second surgical site to harvest the bone, which means additional discomfort and recovery time. However, for large grafts or complex cases, this approach often provides the best results.
Allografts: Donor Bone Options
Allografts use bone from human donors, which is thoroughly processed, sterilized, and tested to ensure safety. This bone comes from tissue banks that follow strict medical standards—similar to organ donation programs.
- Why It’s Common: Allografts eliminate the need for a second surgical site, reducing procedure time and post-operative discomfort. They’re widely used in dental bone grafting and have an excellent safety record.
- How It Works: Though the donor bone doesn’t contain living cells, it provides an effective scaffold for your body to build new bone around.
Xenografts: Animal-Derived Bone
Xenografts typically come from bovine (cow) sources and are processed to remove all organic material, leaving only the mineral structure. This creates a biocompatible material that your body readily accepts.
- Typical Applications: Xenografts are commonly used for sinus lifts and socket preservation. They’re cost-effective, readily available, and integrate well with natural bone.
- Safety Profile: Extensive processing eliminates the risk of disease transmission, making xenografts a safe and reliable option for many patients.
Synthetic Grafts: Modern Alternatives
Synthetic bone grafts are laboratory-created materials designed to mimic natural bone structure. Options include calcium phosphate compounds, bioactive glass, and other advanced materials.
Benefits
Synthetic grafts eliminate any concerns about disease transmission from donor sources and are available in unlimited quantities. They’re particularly useful for patients who prefer not to use animal or human-derived materials.
Use Cases
These grafts work well for smaller defects and routine implant preparation, though some dentists prefer natural materials for more extensive bone regeneration.
Pain, Risks, and Recovery
One of the most common questions patients ask is: “How much will this hurt?” Let’s address the realities of pain management, potential risks, and what recovery actually looks like.
What to Expect During Surgery
Here’s the truth: you shouldn’t feel pain during the bone graft procedure itself. Modern anesthesia techniques ensure you’re comfortable throughout surgery.
Anesthesia Options:
- Local Anesthesia: Numbs only the surgical area; you remain awake but won’t feel pain
- Conscious Sedation: Helps you relax while remaining responsive; you may have little memory of the procedure
- General Anesthesia: Reserved for extensive grafting or patients with severe anxiety; you’re completely unconscious
Most patients describe feeling pressure and vibration during the procedure but no sharp pain. If you do feel discomfort, tell your dentist immediately—they can administer additional anesthesia.
Post-Procedure Healing Timeline
Understanding the recovery process helps set realistic expectations. Here’s what typically happens:
Days 1-3: Expect some swelling, mild to moderate discomfort, and possibly minor bleeding. This is the most uncomfortable period. Ice packs, prescribed pain medication, and rest make a significant difference.
Week 1-2: Swelling decreases significantly. You’ll likely still need to stick with soft foods, but discomfort should be manageable with over-the-counter pain relievers. Your dentist may schedule a follow-up to check healing progress.
Weeks 3-4: Most visible healing occurs during this period. You can gradually return to normal eating, though you should still be gentle around the graft site.
Months 3-6: This is when the real magic happens beneath the surface. Your body is actively building new bone tissue, though you won’t see or feel this process. Your dentist will use imaging to confirm successful bone regeneration before proceeding with implant placement.
The timeline varies based on the graft size, your overall health, and whether you smoke (which significantly delays healing). Following your dentist’s post-operative instructions closely dramatically improves outcomes.
Common Risks and How They’re Managed
Like any surgical procedure, bone grafting carries some risks—but serious complications are rare, especially when performed by experienced dental professionals.
Infection
Occurs in roughly 1-2% of cases. Your dentist will prescribe antibiotics and provide detailed care instructions to minimize this risk. Signs of infection include increased pain, swelling after the first few days, fever, or unusual discharge.
Graft Failure
Sometimes the body doesn’t integrate the graft material as expected. This happens in about 5% of cases and may require repeating the procedure. Smoking, certain medical conditions, and poor oral hygiene increase this risk.
Nerve Damage
Extremely rare but possible if the graft is near major nerves. This can cause temporary or, very rarely, permanent numbness or tingling. Experienced dentists use advanced imaging to plan procedures carefully and avoid nerve structures.
Tips to Minimize Complications:
- Follow all pre- and post-operative instructions exactly as prescribed
- Don’t smoke for at least two weeks before and after surgery (ideally, quit permanently)
- Maintain gentle oral hygiene around the surgical site
- Attend all follow-up appointments
- Report any unusual symptoms immediately
Most patients experience straightforward healing with minimal complications. If something doesn’t feel right, contact your dentist—they’d rather address concerns early than see small issues become bigger problems.
Benefits of Dental Bone Grafting
Now that we’ve covered the process and recovery, let’s discuss why bone grafting is worth considering. The benefits extend far beyond simply preparing for dental implants.
Improving Implant Success
Dental implants have a success rate exceeding 95%—but that success depends heavily on having adequate bone support. A bone graft significantly improves your chances of long-term implant stability.
Increased Stability
Implants placed in grafted bone integrate just as successfully as those placed in natural bone. The graft provides the volume and density necessary for the implant post to fuse with your jawbone.
Longevity
With proper care, dental implants can last 20-30 years or even a lifetime. Bone grafting ensures your implants have the foundation needed to achieve that longevity.
Expanded Options
Sometimes patients are told they “don’t have enough bone” for implants. Bone grafting opens the door to implant treatment that might otherwise be impossible, giving you a permanent tooth replacement option instead of relying on dentures or bridges.
Preserving Facial Structure and Function
The benefits of bone grafting go beyond implant support—they affect your overall quality of life.
Preventing Facial Collapse
When you lose teeth and the supporting bone deteriorates, your face can take on a sunken, aged appearance. The lower third of your face shortens, lips thin out, and wrinkles around the mouth become more pronounced. Bone grafting helps maintain your natural facial contours.
Maintaining Chewing Function
Adequate bone support allows you to eat a full range of foods comfortably and confidently. You won’t need to avoid hard or crunchy foods due to unstable teeth or poorly fitting dentures.
Supporting Clear Speech
Your teeth and jaw structure play a role in how you pronounce certain sounds. Preserving bone health helps maintain clear, natural speech patterns.
Protecting Remaining Teeth
When one area of your jaw loses bone, it can affect neighboring teeth, potentially leading to further tooth loss. Bone grafting stabilizes the area and protects your remaining natural teeth.
If you’re weighing the decision to proceed with a bone graft, consider the long-term benefits to your health, appearance, and quality of life. Consult your dentist to discuss how bone grafting specifically addresses your oral health needs.
Socket Preservation After Tooth Extraction
Here’s a proactive approach that’s becoming increasingly common: placing bone graft material in the tooth socket immediately after extraction. This is called socket preservation or ridge preservation.
Why Timing Matters
Your jawbone begins to shrink within weeks of losing a tooth. By placing a bone graft at the time of extraction, your dentist can minimize bone loss and maintain the ridge shape, making future implant placement easier and more predictable.
The Process
During your tooth extraction, your dentist fills the empty socket with bone graft material and may cover it with a protective membrane or collagen plug. The gum tissue is then sutured closed, and the graft integrates as the extraction site heals.
Benefits
Socket preservation dramatically reduces the amount of bone loss compared to extraction alone. If you’re planning an implant in the future, this approach simplifies treatment and may eliminate the need for more extensive bone grafting later.
Ready to Restore Your Smile’s Foundation
If you’re considering dental implants or have been told you may need a bone graft, the team at U Smile Family Dentistry is here to help. We offer personalized evaluations to assess your jawbone health and determine the best treatment options for long-term success. With advanced techniques and a patient-first approach, we make the process comfortable and easy to understand. Schedule your consultation today and take the first step toward a stronger, healthier smile.
Conclusion
A bone graft for teeth may sound like a complex or intimidating procedure, but in reality, it’s a highly predictable, well-studied solution that helps restore jawbone strength and protect your long-term oral health. Whether you’re preparing for dental implants, addressing bone loss from gum disease, or planning ahead after a tooth extraction, bone grafting creates the solid foundation your smile needs to function and look its best.
With modern techniques, advanced materials, and proper aftercare, most patients heal smoothly and go on to enjoy stable implants, improved facial structure, and renewed confidence when eating and speaking. The key is early evaluation and personalized treatment planning.
Frequently Asked Questions
Is a bone graft for teeth painful?
Most patients report minimal pain during the procedure thanks to local anesthesia or sedation. After surgery, discomfort is usually mild to moderate and can be managed with prescribed or over-the-counter pain medication. Swelling and soreness typically improve within a few days.
How long does a dental bone graft take to heal?
6 Initial gum healing usually occurs within 1–2 weeks, but full bone regeneration takes longer. Most bone grafts require 3 to months to fully integrate before dental implants can be placed, depending on the graft size and your overall health.
Can a bone graft fail?
Bone graft failure is uncommon, but it can happen. Factors such as smoking, uncontrolled medical conditions, infection, or poor oral hygiene can increase the risk. Following your dentist’s instructions closely greatly improves success rates.
Do I always need a bone graft before dental implants?
Not always. Some patients have sufficient bones naturally. However, if bone loss has already occurred due to tooth loss, gum disease, or trauma, a bone graft may be necessary to ensure implant stability and long-term success.
Are there alternatives to bone grafting?
In certain cases, alternatives like shorter implants, angled implants, or different prosthetic options may be considered. However, these aren’t suitable for everyone. A dental bone graft often provides the most reliable and long-lasting foundation for implants.
