A dental crown usually hurts when you bite down because of bite misalignment, nerve inflammation, or an underlying issue beneath the crown. Dental crowns are meant to restore strength, comfort, and normal chewing function, but pain under pressure often indicates that something is not functioning as it should.
Pain like this should not be ignored, even if it feels mild at first. Identifying the exact cause early can prevent further tooth damage, relieve discomfort, and reduce the need for more extensive dental treatment later in Mesa, AZ.
Is It Normal for a Dental Crown to Hurt When Biting?
It is normal to experience mild sensitivity for a few days after getting a new dental crown because your tooth and surrounding tissues are adjusting to the restoration. Slight discomfort when biting or chewing during the first week is generally nothing to worry about.
However, pain that continues beyond a week, worsens, or appears suddenly in an older crown is not normal. Persistent or severe pain can indicate bite misalignment, nerve irritation, or underlying decay, and it’s important to visit your dentist promptly to identify and address the cause.
Common Causes of Crown Pain When Biting Down 
Several factors can contribute to crown pain when you bite down, and this is a common concern for many dental patients. Identifying the specific cause is essential for effective treatment and long-term relief in Mesa, AZ.
High Crown or Bite Misalignment
One of the most frequent culprits behind crown pain is a crown that sits too high. When a crown isn’t properly adjusted to match your bite, it receives excessive force when you chew, leading to discomfort and pressure on the tooth and surrounding structures.
Even a difference of a fraction of a millimeter can cause problems. This issue often occurs immediately after crown placement but can develop over time as your bite naturally shifts. The good news is that bite misalignment is usually one of the easiest problems to fix.
Inflammation of the Tooth Nerve (Pulpitis)
The process of preparing a tooth for a crown involves removing tooth structure, which can sometimes irritate the nerve inside. This irritation, called pulpitis, can cause sensitivity and pain when biting.
In some cases, the inflammation is reversible and will heal on its own within a few weeks. However, if the nerve has been significantly compromised, irreversible pulpitis may develop, potentially requiring root canal treatment to resolve the pain.
Cracked Tooth or Fracture Under the Crown
A crack in the tooth structure beneath the crown can cause sharp, intermittent pain when you bite down. These cracks may have existed before the crown was placed, or they may develop afterward due to trauma, grinding, or normal wear.
Cracks are particularly problematic because they can allow bacteria to enter deeper layers of the tooth and are often difficult to detect on X-rays. The pain from a cracked tooth is typically sharp and occurs when pressure is released rather than when initially applied.
Decay or Infection Beneath the Crown
Although crowns protect teeth, decay can still develop at the margin where the crown meets the natural tooth, especially if oral hygiene isn’t maintained or if the crown doesn’t fit properly. Bacteria can work their way under the crown, causing decay and potentially infection in the tooth or surrounding bone.
An infected tooth often causes persistent, throbbing pain that may worsen when biting. If left untreated, the infection can spread and lead to more serious complications, including abscesses.
Loose or Poorly Fitted Crown
Over time, the cement holding a crown in place can weaken, causing the crown to become loose. A loose crown moves slightly when pressure is applied, which can be painful and allows bacteria to enter the gap between the crown and tooth.
Poor initial fit, cement washout, or decay at the margins can all contribute to crown looseness. You might notice the crown feeling slightly mobile or hear a clicking sound when you bite down.
Gum Irritation or Periodontal Disease
Sometimes the problem isn’t the crown itself but the gums surrounding it. If the crown margin extends too far below the gum line or if there’s inflammation from gum disease, biting pressure can cause pain in the soft tissues.
Periodontal disease around a crowned tooth can lead to bone loss and gum recession, which may cause sensitivity and discomfort when chewing. Proper oral hygiene around crowns is essential to prevent these issues.
Teeth Grinding (Bruxism)
If you grind or clench your teeth, especially at night, you may be subjecting your crowned tooth to excessive force. Bruxism can cause pain in crowned teeth, wear down the crown material, and even crack the tooth beneath the crown.
Many people who grind their teeth aren’t aware of the habit until a dentist points out the signs, such as worn tooth surfaces or jaw muscle tenderness.
Sinus or Referred Pain (Upper Teeth)
Interestingly, pain in an upper crowned tooth might not be coming from the tooth at all. The roots of upper back teeth are located very close to the maxillary sinuses, and sinus infections or inflammation can create pressure that mimics tooth pain.
This referred pain often affects multiple teeth and may worsen when you bend over or lie down. If you have other sinus symptoms like congestion or facial pressure, this might be the culprit.
How to Identify the Source of Pain From a Crown
To identify the source of crown pain, pay close attention to the specific characteristics of the discomfort. Track when the pain occurs, whether it happens only when biting, during consumption of hot or cold foods, or appears spontaneously throughout the day.
Observe the type of pain, noting if it is sharp and sudden or dull and aching. Record how long the pain lingers after pressure or a stimulus is removed, and identify the specific movements, foods, or activities that trigger the discomfort. Keeping detailed notes helps your dentist quickly diagnose the cause and provide the appropriate treatment.
Symptoms Associated With Crown Pain
Crown pain often comes with additional symptoms that help identify the cause. Sensitivity to hot or cold foods and beverages is common, as is a persistent dull ache or throbbing sensation. Sharp, shooting pain can occur when biting down.
Other signs may include swelling or tenderness in the gums around the crown, a bad taste in the mouth, or visible gum discoloration, which can indicate infection. A loose or mobile crown is another important symptom. In severe cases, swelling in the face or a fever may develop, requiring immediate dental attention.
Pain After a Crown — How Long Is Normal and When It’s Not
Some sensitivity for three to five days after getting a new crown is normal as the tooth and surrounding tissues adjust. Mild discomfort when biting during this period is usually not concerning, especially if it gradually improves.
Pain that persists beyond two weeks, increases in intensity, or appears suddenly after a period of normalcy is abnormal and requires evaluation. New pain in a crown that has been in place for months or years should always be checked by a dentist. Trust your instincts—pain that interferes with eating or daily comfort should not be ignored.
How Dentists Diagnose Crown Pain
Dentists begin with a comprehensive examination and discussion of your symptoms. They visually inspect the crown and surrounding tissues for cracks, decay, or gum inflammation. Bite tests are performed to check for high spots or specific areas causing discomfort.
X-rays are used to detect issues beneath the crown, such as decay, infection, or bone loss, though some cracks may not appear. Dentists may also test the tooth’s response to temperature or gentle tapping. In certain cases, advanced imaging, such as a cone beam CT scan, provides a more detailed view of the tooth and surrounding bone.
How Dentists Treat Crown Pain When Biting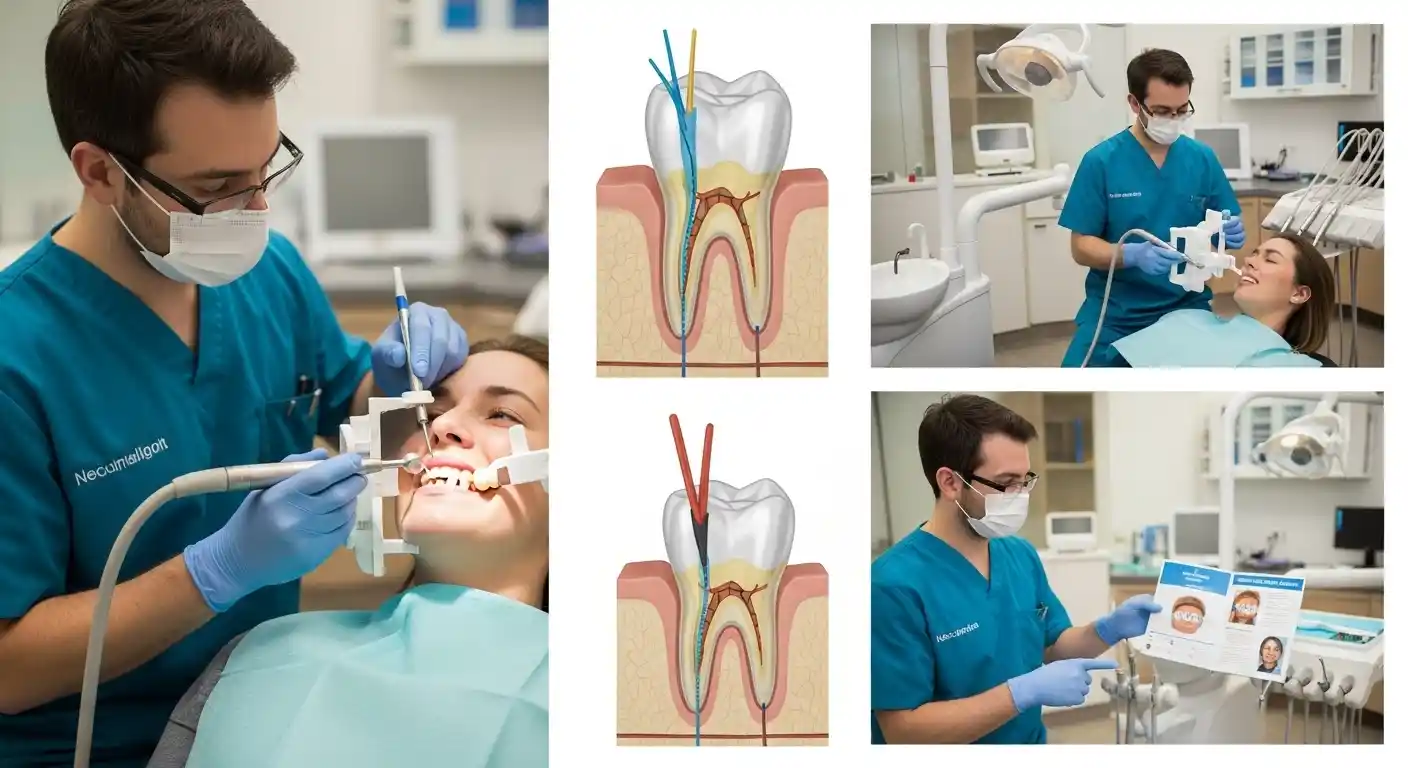
Treatment depends entirely on the underlying cause of your pain. Your dentist will develop a plan tailored to your specific situation.
Bite Adjustment
If your crown is sitting too high, your dentist can adjust it by carefully removing small amounts of material from the crown’s biting surface. This is usually a quick, painless procedure that provides immediate relief. Your dentist will use special marking paper to identify high spots and will make precise adjustments until your bite feels comfortable and even. Multiple appointments may be necessary to fine-tune the adjustment.
Crown Re-cementation or Replacement
A loose crown can often be cleaned and re-cemented if the tooth underneath is still healthy. However, if there’s decay beneath the crown or if the crown is damaged, replacement will be necessary. Your dentist will remove the old crown, treat any underlying issues, and fabricate a new crown that fits properly. This process typically requires two appointments, though same-day crowns are available in some dental offices.
Treating Infection or Decay
If decay or infection is present, your dentist must remove the affected tissue before any other treatment can proceed. This might involve removing the crown, cleaning out decay, and potentially placing a filling or build-up before re-crowning the tooth. Antibiotics may be prescribed if there’s an active infection, though they address symptoms rather than cure the underlying problem. Definitive treatment requires removing the source of infection.
Root Canal Treatment
When the nerve inside the crowned tooth is infected or irreversibly inflamed, root canal treatment becomes necessary. This procedure removes the damaged nerve tissue, cleans and disinfects the interior of the tooth, and seals it to prevent future infection. While root canals have an intimidating reputation, modern techniques and anesthesia make them comparable in discomfort to getting a filling. After root canal treatment, the existing crown can often be retained, though some cases require crown replacement.
Night Guard for Teeth Grinding
If bruxism is contributing to your crown pain, your dentist will likely recommend a custom night guard. This dental appliance fits over your teeth and protects them from grinding forces while you sleep. Night guards distribute pressure more evenly and can significantly reduce pain and prevent further damage to your crown and natural teeth. Custom guards made by your dentist fit better and last longer than over-the-counter options.
Home Care Tips While You Wait for Your Dental Appointment
While waiting to see your dentist, there are several ways to manage crown pain and reduce discomfort. Avoid chewing on the affected side and stick to soft foods that require minimal pressure. Over-the-counter pain relievers, such as ibuprofen, can help reduce inflammation and pain when used according to instructions. Rinsing with warm salt water several times a day can soothe irritated gums.
Avoid very hot, cold, or sweet foods that may trigger sensitivity. If you grind your teeth and do not have a night guard, try to stay aware of clenching during the day and consider using a temporary over-the-counter guard. Maintain oral hygiene by brushing gently and flossing carefully around the crown to keep the area clean without causing additional irritation.
When to See a Dentist for Crown Pain
Prompt dental attention is necessary for certain types of crown pain. Severe or persistent pain that does not respond to over-the-counter medication, swelling in the face, gums, or jaw, or a loose crown all require an urgent dental visit. Pain accompanied by a fever may indicate a spreading infection that needs immediate treatment.
Any crown pain lasting more than a week should be evaluated by a dentist. Even manageable pain benefits from early intervention, which can prevent more serious complications and often allows for simpler, less expensive treatment.
Prevention Tips to Avoid Crown Pain in the Future
Proper care of your crown helps prevent pain and extends its lifespan. Brush twice daily and floss carefully around the crown, and attend regular dental checkups to catch issues early. Use a night guard if you grind your teeth, and avoid biting hard or sticky foods that could damage or dislodge the crown. Report any changes in how your crown feels promptly to your dentist, as even small bite issues can lead to discomfort over time.
Crown pain is usually treatable once the cause is identified. Whether it is a minor bite adjustment or a more complex issue like an infection, early intervention allows for effective treatment and prevents more extensive procedures later.
Protect Your Crown and Maintain a Healthy Smile
Take control of your dental health and protect your smile. Schedule regular checkups with our Mesa dentists, maintain excellent oral hygiene, and use a night guard if you grind your teeth. Avoid hard or sticky foods that can damage your crowns and ensure long-lasting comfort and function. Act today to keep your smile healthy and pain-free for years to come.
Conclusion
Crown pain when biting down can be uncomfortable, but it is almost always treatable once the cause is identified. Mild sensitivity after a new crown is normal, but persistent, sharp, or worsening pain requires prompt attention from your dentist. By understanding the common causes—such as bite misalignment, nerve irritation, decay, or bruxism—you can take proactive steps to protect your crown and maintain a healthy smile. Regular dental visits, proper oral hygiene, and early intervention are key to preventing complications and ensuring long-lasting comfort and function. Don’t ignore discomfort; addressing it early can save you time, money, and unnecessary pain.
Frequently Asked Questions
Is it normal for a new crown to hurt when biting?
Yes, mild sensitivity for a few days after crown placement is normal as your tooth and gums adjust. Pain that persists beyond a week or worsens should be evaluated by a dentist.
What causes a crown to hurt when biting down?
Common causes include a high crown or bite misalignment, nerve inflammation (pulpitis), cracked teeth, decay beneath the crown, gum issues, and teeth grinding (bruxism).
How can I relieve pain from a crown at home?
Manage discomfort by avoiding chewing on the affected side, eating soft foods, using over-the-counter pain relievers, rinsing with warm salt water, and maintaining gentle oral hygiene around the crown.
When should I see a dentist for crown pain?
Seek dental care immediately for severe or persistent pain, swelling, fever, or a loose crown. Any crown pain lasting more than a week should be evaluated to prevent further complications.
How can I prevent crown pain in the future?
Proper oral hygiene, regular dental checkups, using a night guard if you grind your teeth, and avoiding hard or sticky foods can help protect your crown and maintain long-term comfort.
